Obstructive Sleep Apnea (OSA) Treatment
View and download the Fact Sheet below.
View and download the Fact Sheet below.
View and download the Fact Sheet below.
Winston
Yes, I am aware of the national TV ads for the hypoglossal nerve stimulator for Obstructive Sleep Apnea. Earlier this year I prepared an information sheet on the subject. I will add it to this letter.
It is a second line therapy and works for a limited sub group of patients with Obstructive Sleep Apnea. CPAP is far more successful in controlling sleep apnea.
It primarily indicated for those who have failed CPAP. Unfortunately, there is no accepted definition what constitutes failing CPAP therapy. Reasons for stopping CPAP are many and sometimes complex. I have been intrigued by the issues that cause a patient to discontinue or be unable to use it and will add more on the subject on another occasion.
RGH 29.112
Sept 2023
“Inspire” is a device that senses an obstructive apneas and then sends a signal to the hypoglossal nerve through a wire. It activates the nerve, which causes the base of the tongue to move forward. The device, wires that sense the apnea and the wire from the device to the nerve are implanted under the skin. It is remotely controlled.
Its primary indication for use is failure to be able to use CPAP. Problems with insomnia, restless legs or other sleep disorders must be controlled before being considered for Inspire. The obstructive apnea rating (apnea hypopnea index or AHI) on diagnostic testing should be between 15 and 65. Weight should be a BMI of under 32. BMI varies by height. For a 5’11” person a BMI of 32 is 225 lbs. Some insurances will allow a slightly higher BMIs. You must be older than 18 years of age. It is indicated when apnea obstruction occurs at the base of the tongue.
A rough estimate of the cost of the device, its implantation, testing and physician visits will be between forty and fifty thousand dollars.
“Inspire” is a second line therapy and insurance companies only approve those who have failed other forms of treatment.
If you meet the criteria for the device, you will be evaluated to see if the device will correct your apnea. The evaluation steps include a facility based sleep study, a sedated endoscopy of your upper airway and provider visits. Many will not fit the type of obstruction that the device will correct and will not be candidates.
If you are a candidate, then implantation, physician review and repeat testing to insure appropriate function will be required. These steps include surgery, a post activation facility based sleep study and provider visits.
The overall time from initial consideration to successful activation is about 5 to 6 months. Medical follow up currently is recommended every 6 to 12 months.
The goals of treating obstructive apnea are to reduce the AHI to less than 5 and to improve the quality of sleep. CPAP will achieve AHIs < 5 a very high percentage of the time. The Inspire device will reduce the AHI to less than 5 in approximately 50% of recipients. The rest will have a reduction in their AHIs but not to normal levels. Standard therapies such as CPAP may still be needed.
“Inspire” is a man-made product with batteries. Wires can break. Wires cannot easily be removed. Batteries or new wires may be required in the future. There are a limited number of experienced physicians available to deal with the device. Other devices may still be needed and recommended to control your apnea condition.
It is inspiring to learn of your interest in sleep apnea. I will be happy to do my best to simplify, clarify and muddy your understanding of the AHI. AHI stands for Apnea Hypopnea Index. It is the standard for defining the presence of significant sleep disordered breathing and the condition of Obstructive Sleep Apnea.
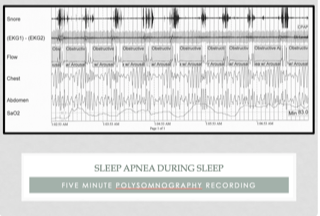
It started long ago in the history of sleep medicine. In actual time, it was just 40-50 years ago. Physicians noted breathing problems during sleep. Over a decade or so it was clear from investigations that the problem was one of blockage of the airway in the throat during sleep. The blockage resulted in less air getting in and out of the lungs. The blood oxygen levels would drop, while the carbon dioxide level would increase. The sleeper responded with increased breathing efforts, which opened the airway. By the 1980’s, testing for these variables had evolved from investigative to the clinical practice level.
The AHI is the fundamental measurement for obstructive and central types of sleep disordered breathing. The A stands for apnea, or absence of breath. The H stands for hypopnea, or a critical reduction of airflow causing the same physiologic changes that the apnea produces. The I stands for index but actually represents a measurement of rate, the number of apneas and hypopneas per hour of sleep. The apnea as used in AHI represents the absences of air movement at the nose and mouth. Respiratory efforts by the diaphragm and chest may or may not be present. These are the simple definitions.
Clinicians and physiologists have much more specific definitions. Our definitions include the magnitude and duration of physiologic changes, as well as the types of equipment used for the measurements and the frequency of the changes. It should not surprise you that significant debate continues about the details of those changes. Opinions differ. Unfortunately, the efficient computerized testing systems we utilize, ease the burden of testing large numbers of people, but limit the ability to look at multiple variations of potential changes in definitions.
In this country, current technical definitions and the threshold for diagnosing the medical condition of apnea are cemented in place by the regulatory bodies; Medicare and commercial insurance companies set the standards. While the definitions set are supported by reported evidence, the standards are far from perfect and will not change soon.
The AHI is the gold standard for the definition of obstructive and central sleep apnea. Five events, apneas and or hypopneas, per hour of sleep meet diagnostic level for apnea. The level of 5 events was arrived at arbitrarily, based on early work in the field. Although accepted by those regulating groups, the actual minimal AHI needed to establish the diagnosis is not really known.
It is known that the higher the AHI the greater the risk for long-term medical problems. When a sleep study is complete and the AHI criteria for apnea is met, it is described as mild (5-15 events}, moderate (15-30 events) or severe (>30 events) apnea. The adjectives (mild, moderate and severe) represent the long-term risk for medical complications, not how a person feels. These separations into different severities of apnea, represent more tradition than science. In fact, the AHI is only a good predictor of severity for long-term complications at high levels (more complications) and very low levels (less complications). In the decades since these definitions for the onset and the severity of the disease were adopted, much research has been done. It appears that further definitions of these obstructive events would improve the accuracy of our diagnoses and the predictability of the future for the patient.
The current definitions have served time well. As a clinical tool, the AHI has proven to be extremely useful. It is accepted worldwide. Tremendous improvement in diagnosis and therapy for sleep apnea has occurred utilizing these measurements. There are limitations, however. This is specifically true when scientific studies of the condition are performed.
The role of low oxygen levels has been investigated more than any other factor. You will recall oxygen is measured on testing by the noninvasive transcutaneous method that reports oxygen saturations. Our technical definitions include a certain drop in oxygen saturation that is caused by the interruption to the airflow during the breathing events. The roles of the duration, severity and timing of the drop of oxygen in the sleep pattern as well as the total time spent at certain levels of oxygen desaturation are not known. Studies reviewing low oxygen levels during apnea suggest that the time spent with saturations of less than 90% together with the AHI is more accurate in predicting long-term medical complications than the AHI alone.
Another major factor not addressed with current testing is the use of a rate measurement for diagnostic purposes. A rate does not measure total exposure to apnea events. That is dependent on actual sleep time. An easy example is the difference of someone sleeping six hours versus another person who sleeps nine hours. They both can have the same AHI, but the person sleeping nine hours will be exposed to 50% more apnea events than the person who only sleeps six. The importance of exposure has not been studied at all.
The events we measure, apneas and hypopneas, do not occur uniformly throughout a night of sleep. The event frequency can change based upon body position. They can occur more while sleeping on the back verses the stomach. The events can occur more in REM sleep than in slow wave or Non-REM sleep. Research into the effects of these variables as predictors of long-term outcomes is limited.
Well, I believe it is time to close. The AHI is an immensely useful tool in the diagnosis and treatment of sleep apnea. It is the gold standard measurement for the diagnosis of sleep apnea. It needs to be improved upon and will be. As you will learn throughout your career, medicine changes slowly. Opinions are more rigid in medicine and in science than most believe. So, keep an open mind. This, like all things medical, will change with time.
RGH 7 April 2023 (28960)

Winston Oct 29, 2022
Yes, I will try to answer your question. I understand your training has led you to believe that healthcare is a right. Why, you ask, did I pause before saying, “It’s not that simple. But if it were, the answer would have to be no.”
Consider first what is meant by the term, healthcare. Like most words, it is likely interpreted differently by almost everyone. The views will run from having clean water, a family doctor available for medical problems to those that would include anything to do with a person’s health. These are widely divergent categories of products and services based on different delivery systems and business models. It is almost impossible to discuss a ‘right to healthcare’ without understanding everything that is included in the discussion – the components of healthcare.
It is not the only term that needs to be defined. What do the promoters mean by the word, right? Maybe it is best to consider its meaning first.
When right is used as a noun, as it is in a ‘right to healthcare,’ common definitions according to Merriam-Webster include: qualities of moral correctness or moral propriety; something to which someone has a just claim; something to which someone may claim as their due; and, a cause of truth or justness. The proponents of a ‘right to healthcare’ usually mean the second or third of these definitions, a just claim or their due.
Healthcare has only one definition listed. Merriam-Webster defines it as ‘efforts to maintain or restore physical, mental or emotional well-being especially by trained or licensed professionals.’ Practically speaking, this definition would essentially cover all aspects of personal and public health. It would include the fields of preventive medicine, public health and personal medical care along with institutional medical care. Each of these fields is unique in how it is currently organized and delivered while sharing some common features. The shared features include the need for physical plants of operation, equipment to provide the services, support staff to carry out the services and a professional staff. These factors are needed in varying quantities and of different types for each of these fields of endeavors.
For clearer understanding we need to look more specifically at the services included in healthcare. These would include public health services, preventive medicine services (public or individual), individual’s urgent and chronic medical care, and institutional care (hospitalization and similar). We need to consider all the services that might be determined to be healthcare.
Public health is widely practiced throughout most local communities in our country. Public health services maintain and ensure clean water and adequate sewers, track communicable diseases and advise the population about those diseases. Their services, physical plant, equipment, staff and professionals are paid for and employed by government units. They are paid for by taxes and by fees for water and sewer services. For the majority of urban areas in this country, these health services are for all practical purposes already a right provided by the government. Certainly, there are exceptions for rural and smaller communities, but most citizens already enjoy public health as a government service. Paid for by their taxes.
Preventive medical services are currently provided by both government operations and individual medical providers. Examples of government services include monitoring of new and current medications for problems, providing recommendations for vaccinations, and monitoring of medical devices. Again, the facilities, staff, equipment and professionals are supplied and paid for by the government taxes and fees usually paid by the businesses for the service.
At a more personal level, physicians, providers, healthcare businesses and employers (insurance companies, medical practices, clinics, hospitals and businesses) may provide guidance and assistance on preventive medical measures that an individual needs. These businesses provide the physical plant, staff, equipment and professional organization needed. The expense for these services is recouped through fees, insurance payment, employers and other methods. The healthcare provided at this level is the first at which an individual may be responsible for all or part of the cost of the services.
The next component leads further into individual responsibility, providing an individual’s urgent and ongoing medical care. This is the form of healthcare we are familiar with and what is most often thought of when discussing ‘a right to healthcare’. In our country’s history, these services have been provided by individual professionals who own and operate their own businesses. Recent change in economics, economic policy and legal structures of medical businesses has led to more large organizations (hospitals and insurance companies) owning more of these types of businesses. In these operations in any form, the expenses – from cotton swabs to physician income – are paid for by individuals, either directly or through surrogates (employers, insurances or others).
An individual’s surrogates are the primary payees for the institutional care portion of our healthcare delivery system. This portion of healthcare, hospitalization primarily, is where the largest cost (facilities, equipment, staff and professionals) occurs. Again, most of the cost is paid for by individuals or their surrogates.
In these areas of healthcare where the individual is mostly responsible for the cost of the service, there is one major group of individuals that is not responsible directly. Those are individuals on government insurance such as Medicare. In Medicare and other government plans, a person may have a markedly reduced or no exposure to the direct cost of the services. Those who argue for a ‘right to healthcare” would like all services for all citizens to be paid for by the government.
My comments have gone on long enough so I will save my additional thoughts for a future letter. I would add in closing what I think summarizes the whole question.
A ‘right to healthcare’ should mean everyone has access to and freedom to decide how to obtain their healthcare. At present, I would argue that it is already the case, but it is disappearing rapidly. In reality, the discussion is not about freedom to get healthcare, but getting healthcare for free.
RGH
28,775